Colistin in the Modern World
- symthasreeskoganti
- Apr 7, 2025
- 3 min read
Fairfax, VA
Edited by Elin S.
We live in an era of rising antibiotic resistance, one where superbugs or multidrug-resistant (MDR) bacteria have begun to emerge, posing a threat to us all.
Once sidelined due to concerns of toxicity, it could now be used as a new defense against MDR strains. Posing a heavy concern to public health, these strains are difficult to treat due to their resistance, causing longer hospital stays, higher healthcare costs, and increased mortality rates. Yet, as colistin’s promise of potential grows, so do the challenges associated with it. Thus, one may ask: What role does colistin now hold in our modern world?

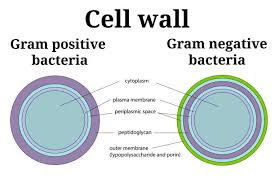
To understand colistin’s place in the present, we must first get to know its past. Colistin was discovered in 1947 Japan from Paenibacillus polymyxa subsp. colistinus cultures and was found to be effective against most harmful gram-negative bacteria. Gram-negative and gram-positive bacteria are differentiated by the former’s type of outer membrane, consisting of a peptidoglycan cell wall between two membranes with lipopolysaccharides. It is these very lipopolysaccharides that colistin targets. By binding to lipopolysaccharides, this antibiotic causes the outer cell membrane to release them and thus alters permeability. Colistin takes advantage of this to access the inner membrane and disrupt it, gaining entry into the gram-negative bacteria.
The US FDA approved colistin for use against gram-negative bacteria in 1959 and was first clinically used as an intravenous injection (given through the veins). This clinical use, however, was short-lived (lasting only until the 1970s) with the discovery of the antibiotic’s toxicity to the kidneys and nervous system. Its only main use that continued was for cystic fibrosis patients, as colistin was a helpful treatment against those infected with Pseudomonas aeruginosa. Newer and safer antibiotics had been researched at this point, such as cephalosporins and penicillins, and overall patient outcomes would benefit from these options being used instead. Yet in the 1990s, colistin again re-emerged to be used against MDR bacteria that had become resistant to the large majority of antibiotics in use at the time. It is worth noting that colistin had not become any safer over those two decades, emphasizing the true last resort it was in treatments.
In the modern day, we still struggle to deal with such MDR pathogens, which can take what would have been a common infection into a treatment struggle. Colistin, with its resurgence, has been under research scrutiny to make it safer —with approaches ranging from different dosings to modification of the medication itself. It is currently only available in the forms of colistin sulphate (to take orally) and colistimethate sodium (given as injections due to its weaker toxicity than colistin sulphate). Some studies, though on small scales, have shown that colistimethate sodium combination therapy (providing this form of colistin in combination with another antibiotic) could lead to better outcomes for the patients. However, as these studies have not been conducted on a larger scale, the extent of a clinical advantage is uncertain.
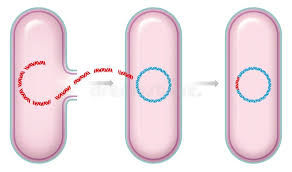
If safer administration of colistin is to be discovered, then it must be found soon. A 2015 paper by Liu et al. details the first colistin-resistance gene that can be transferred between different bacteria. The gene was named mcr-1 as shorthand for mobile colistin resistance-1, was identified in was E. coli strain SHP45. Through a process called horizontal gene transfer, bacteria may spread such colistin resistance to other non-offspring bacteria. The infrequent use of colistin had thus far prevented such resistances from developing, unlike the case of many commonly used antibiotics. However, with the resurgence of colistin as a last-resort treatment, the development of resistance was inevitable. Research efforts will continue to pursue colistin’s potential while undergoing the lengthy process of discovering new antibiotics—but the approach to overcoming MDR pathogens is yet to be discovered.
Sources:
Enjoyed this? Check out more of our content:














Comments